Background:
In recent years, wider use of hydroxyurea has increased the average lifespan of individuals with sickle cell disease (SCD). With increased lifespan, recent reports suggest an increase in the risk of malignancy in SCD patients. Studies from California report a 72% increased risk of developing hematologic malignancies in patients with SCD compared to age, sex, and race matched controls. However, cancer-specific survival is similar to non-SCD patients. There are no guidelines for treatment considerations in the management of malignancies in patients with SCD. Therefore, we surveyed adult and pediatric SCD providers on their approaches to the management of cancer in patients with SCD. Herein we present preliminary data from the initial survey respondents.
Methods:
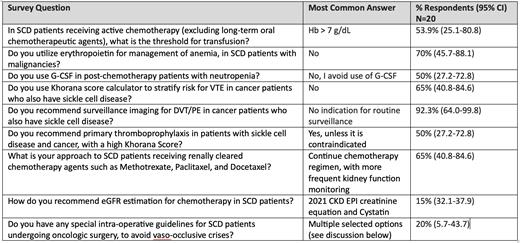
Adult and pediatric SCD providers were invited to participate in an electronically distributed REDCap survey. This survey contained 18 questions designed to determine practice preferences in the provider's approach to management of malignancies in patients with SCD, including the management of anemia, anticoagulation, and peri-operative considerations. The responses to each survey question were analyzed for trends, with responses summarized in counts, percentages, and corresponding 95% Clopper-Pearson confidence intervals (CI).
Results:
Among 47 providers that have completed the survey to date, 20 have managed patients with co-existing SCD and malignancies and were included in the analysis. In this provider group, which included both physicians and advanced practice providers, half [50% (CI 27.2-72.8)] care for 200-500 patients with SCD annually. The most common survey responses to selected questions are summarized in Table 1.
Conclusion:
Comprehensive care for patients over the last few decades has increased the lifespan of people living with SCD. This has resulted in an increased diagnosis of adult-onset cancers along with associated challenges in cancer management.
Thus far, the survey responses have shown a trend that providers maintain a hemoglobin goal of 7 g/dL for transfusions, and the majority do not use erythropoietic stimulating agents for the management of anemia. Most providers reported not using G-CSF in post-chemotherapy neutropenic patients. When asked about primary thromboprophylaxis, responders said they do not routinely use the Khorana score for risk stratification or recommend surveillance imaging for venous thromboembolic events [VTE]. However, if the Khorana score is high or patients are on thrombogenic agents, providers recommend consideration of primary prophylactic anticoagulation. Providers also recommend close monitoring of renal function with the use of renally cleared chemotherapy agents. Multiple methods such as the use of Bair Huggers, warming blankets, warm IV fluids and avoidance of cell savers, tourniquets and intra-operative fluoroscopy were recommended to avoid peri-operative vaso-occlusive crisis. These data are limited currently, with insufficient responses to conduct larger analyses. Given the paucity of clinical data and the nuances associated with sickle cell specific risks, there may be reliance on expert opinion for the management of malignancies in patients with sickle cell disease.
Disclosures
Desai:POC Detection of Hemoglobin Sickling via Magnetic Fractionation: Patents & Royalties: (Pending); US Food & Drug Administration: Research Funding; University of Tennessee: Research Funding; University of Pittsburgh: Research Funding; PCORI: Research Funding; NIH: Research Funding; Novartis: Research Funding, Speakers Bureau; Chiesi: Consultancy; Vertex: Consultancy; Forma Therapeutics: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal